Paraparesis- a case study
Three scenarios
of paraparesis:
Three different cases have been allotted of paraparesis in a 23M and two 18yr old
males. This is my attempt in understanding the patient’s priorities regarding
his symptoms and understanding and suggesting investigations and treatment
options for the same.
CASE 1
The
following is a case of a 23M, an auto driver by occupation, who came with
bilateral weakness of lower limbs.
https://vaish7.blogspot.com/2020/05/medicine.html?m=1
these are the important symptoms of the patient:
these are the important symptoms of the patient:
- Weakness in both lower limbs since 5 days
- Tingling and numbness
- Vomiting 5 days ago ( increased ICP)
History of
presenting illness:
Patient was
apparently asymptomatic 5 days back, then developed weakness of both lower
limbs associated with tingling and numbness in the limbs. He said that he
suddenly fell down when he got up to urinate and was helped up by his father.
He has H/O vomiting which was non projectile, non-bilious, contents being food
particles, 3-5 episodes.
Past
history:
H/O multiple
sexual partners (could be an STD)
H/O
operation for gluteal abscess 5 months back and incision and drainage of
scrotal abscess 10 days back.
Family
history:
Non-significant
On general
examination: everything appeared normal
On
examination of motor system:
- Hypotonia in both lower limbs (LMN)
- Reduced power in both lower limbs (LMN)
- Babinskis sign positive (UMN) S1-2
- Exaggerated reflexes (UMN)
- Ankle clonus is present in right (UMN)L4-5
- Primitive reflex is absent (LMN)
- Involuntary movements are absent
Meningeal
signs are negative
Investigations:
- Lymphocytes are increased
- On MRI: There is ring enhancement which could be due to meningeal enhancement or exudates
- Lesions in MRI with multiple nodules seen in the pulmonary apices suggestive of pulmonary Koch’s and disseminated TB
- On abdominal x ray, left psoas abscess was identified.
- ESR raised- could be due to cranial arteritis
- serology is negative
Describing the
complaints of the patient we have:
-Weakness of
both lower limbs with tingling and numbness:
- Weakness can be categorized under various etiologies but on history and examination, gluteal abscess (drained 5 months ago) and scrotal abscess (drained 10 days ago) could be suggestive of an infectious etiology of the bilateral lower limb weakness
- Motor system examination revealed hypotonia, loss of power, reflexes present and ankle clonus absent.
- hypotonia is suggestive of LMN lesion and the rest suggest UMN lesion.
- Meningeal signs were all negative, that is, kernigs sign, brudzinkis sign, or neck stiffness. so it is not infectious meningitis.
- routine x ray revealed multiple apical nodules which could be suggestive of disseminated tb.
- Potts disease to be excluded as there is TB associated with paraparesis, especially in thoracic spine disease.
- Also x-ray abdomen revealed a psoas abscess on the left which could be compressing nerves supplying the lower limbs. In such case, reflexes should be absent which is not the case. Hence LMN lesion is not what caused the paraparesis.
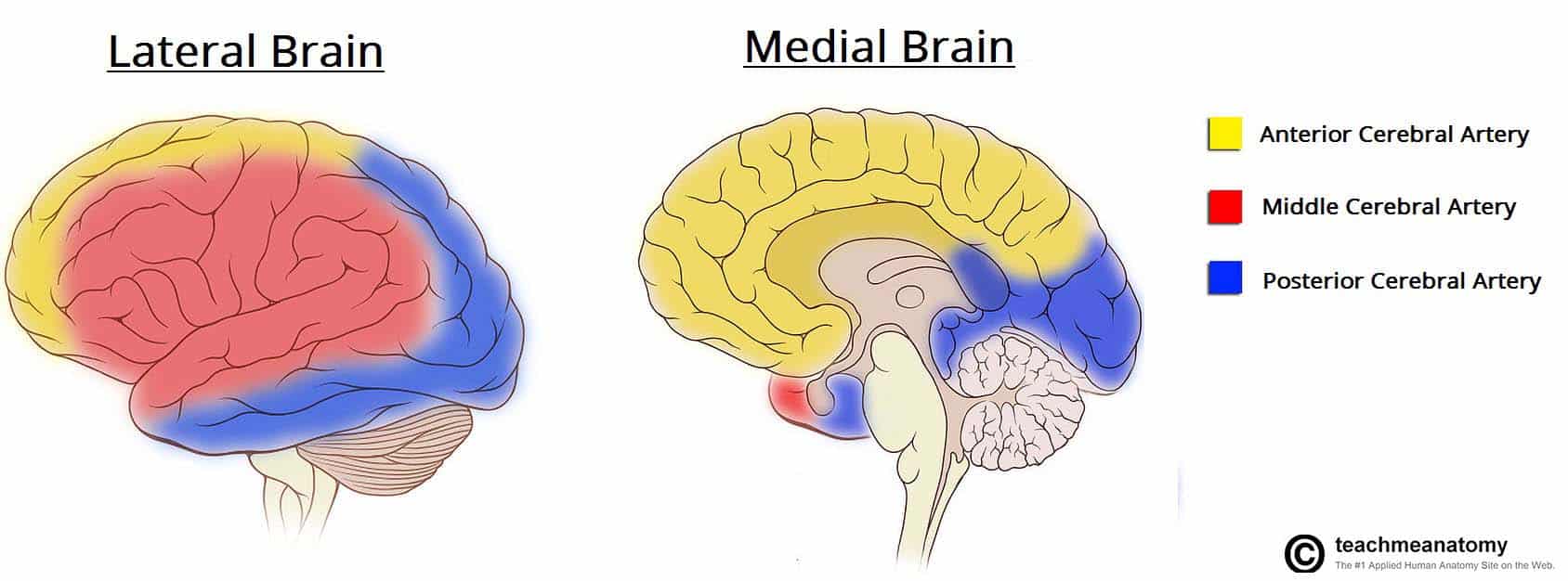
- On MRI brain, enhancement was observed in the medial and lateral brain in the frontal and parietal lobe regions essentially in the region supplied by the anterior cerebral artery as seen in the image below. The enhancement is more on the medial brain which is the region supplying the lower limb. Hence the lesion can be the reason for the paraparesis. The enhancement showed bilateral appearance suggestive of a vascular origin of the lesion, vasculitis, as indicated by the raised ESR.

- tingling and numbness can also be attributed to the brain lesion.
-Vomiting:
This could
be due to the raised intracranial pressure attributed to the lesion seen on the
MRI brain.
other investigations that can be done:
other investigations that can be done:
- MRI spine
- Culture and sensitivity of the evacuated pus from the gluteal and scrotal abscess
References:
- Dr. vaishnavi's log
- https://teachmeanatomy.info/neuroanatomy/vessels/arterial-supply
- https://www.pinterest.com/pin/548876273312302344/
- https://www.healthline.com/symptom/muscle-weakness#caus
- https://medicinedepartment.blogspot.com/2020/05/frequently-asked-questions-around-case.html?m=1
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3691413/
- Davidson's principles and practice of medicine
CASE 2
the next case is of an 18 yr old male with complaints of difficulty in walking
the important
symptoms presented by the patient:
- difficulty
in walking since 1 month
- bilateral
lower limbs weakness since 1 month
- pain
in the lower limbs calf muscles since 1 month.
- H/o
pain in the calf muscles while walking/calf tender positive.
- H/o
difficulty in standing from sitting position.
- H/o
difficulty in climbing stairs
- H/o
difficulty in holding chappals
- H/o wasting and thinning of muscles (LL>UL)
- Muscle bulk has been reduced in all the limbs initially
- There is hypotonia and power of the lower limbs is reduced. Deep tendon reflexes are absent and plantar reflex is also absent.
- This suggests a lower motor neuron lesion causing paraparesis.
- Lesions of scabies seen in the web spaces or the hands which was acquired through his group of members. there was no itching and serology was negative.
- Nerve conduction studies revealed bilateral common peroneal and sural axonal neuropathy
- Sural nerve biopsy planned
References:
- Dr. Hitesh's log
- Davidson's principles and practice of medicine
CASE 3
The next case is of a 18yr old male with complaint of bilateral lower limb weakness since 20 days
important symptoms presented:
- weakness of both lower limbs begining with the proximal region, gradually progressive over 2 yrs
- difficulty in getting up from a squatting position
- difficulty in wearing and holding chappal
- bilateral non pitting type of edema
on examination, there is
- Loss of power
- Absent reflexes in LL
Absence of loss of tone makes us think that it is probably
not involving the nerves so it is not a neuropathy but a myopathy
muscle biopsy result suggested polymyositis or muscular dystrophy
- "Polymyositis (pol-e-my-o-SY-tis) is an uncommon inflammatory disease that causes muscle weakness affecting both sides of your body. Having this condition can make it difficult to climb stairs, rise from a seated position, lift objects or reach overhead."- Mayo clinic
- "Muscular dystrophy is a group of diseases that cause progressive weakness and loss of muscle mass. In muscular dystrophy, abnormal genes (mutations) interfere with the production of proteins needed to form healthy muscle" - Mayo clinic
Suggested investigations:
- genetic testing for DMD gene
- test for serum ANA to rule out autoimmune conditions
References:
Comments
Post a Comment